By Lindsey Wimmer, MSN, CPNP, CPLC
Umbilical cord accidents continue to be the number one topic I hear about in emails and phone calls from pregnant or grieving families. The reasons for this are many. I do not claim to be an expert on umbilical cord issues, and the topic has been poorly researched. However, I struggle with the ‘facts’ that are often used without telling the whole truth. Here is my understanding of the most common questions or comments I hear regarding cord accidents.
The Whole Truth
 It is true that a significant number of babies are born with cords around their necks and the majority of them do not show any signs of distress. This does NOT mean, however, that cords cannot cause problems! To tell someone that cords can’t be problematic because they aren’t ALWAYS problematic is misleading.
It is true that a significant number of babies are born with cords around their necks and the majority of them do not show any signs of distress. This does NOT mean, however, that cords cannot cause problems! To tell someone that cords can’t be problematic because they aren’t ALWAYS problematic is misleading.
Not EVERY person who smokes tobacco will die of lung cancer. Does this mean smoking doesn’t cause lung cancer? Of course not. Does it mean we don’t need to tell people who smoke of the dangers? Of course not.
If your baby was born with an umbilical cord issue and your baby is happy and healthy, PLEASE count your blessings and consider yourself fortunate to have landed on that side of the statistics. We are not all so lucky. Most of all, please don’t say my baby’s cause of death isn’t significant or worth worrying about just because it didn’t happen to your baby.
Should I worry about the ‘nuchal’ cord?
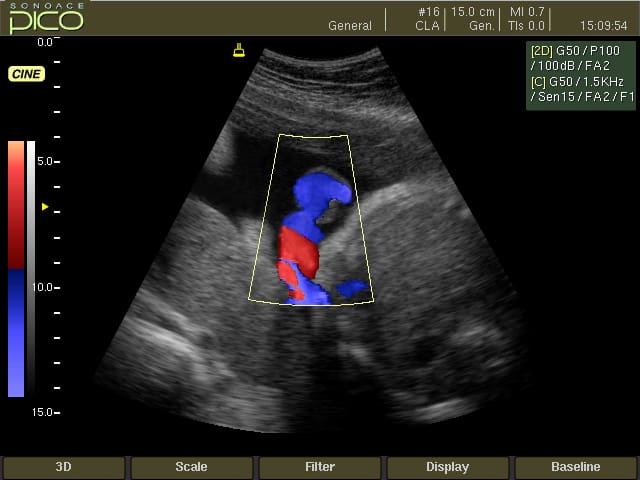
When we hear about cord issues, most people think about or are talking about nuchal cords. This is when the umbilical cord is wrapped around the baby’s neck. That placement alone is not necessarily the problem. It is a problem if it is wrapped tightly. However – not for the reason most people think. A tightly wrapped nuchal cord is not a concern because of the baby’s neck (before birth, the baby does not get oxygen through the trachea into the lungs). It is a concern because of the compression that is put on the cord itself. The umbilical cord IS how the baby gets oxygen before birth. So – a nuchal cord that is tight enough to restrict blood flow through the cord between the placenta and the baby puts the baby’s oxygen supply at risk. However – the same is true for any position of the baby and umbilical cord that compresses the cord and reduces blood flow. This can occur around a limb, around the baby’s body, as a knot in the umbilical cord, with multiple nuchal cords or wraps, as a poor insertion point into the placenta, between the baby’s body and mom’s, and so forth. Nuchal cords get the most attention, but that is just one type of potential cord issue.
My doctor says cord accidents don’t cause problems and then my doctor said my baby was stillborn due to a cord accident.
I am the first to admit that the research into umbilical cord issues and how to manage them is lacking. Much more is needed. But the problem is compounded by the medical community not even being able to agree if this is a legitimate cause of death. The part that is most frustrating to me is that many providers use both of the above statements when it fits the situation.
According to the Stillbirth Collaborative Research Network (SCRN) studies, 11% of all stillbirths were determined to be caused by umbilical cord issues. By their own description, this is probably a low number because they had very strict conditions for coming to this conclusion and required definitive pathologic evidence of such.
It can be extremely distressful and frustrating to parents to hear during the pregnancy that umbilical cords don’t cause problems and then after the pregnancy that the cause of their baby’s death was an umbilical cord accident. We can’t have it both ways. This gives the appearance that providers either don’t know about the issue or they are taking the “easy” way out. (Meaning it’s easier to reassure parents and play the odds during the pregnancy.) It’s also easier after a stillbirth to provide an “answer” that is easy for families to understand and accept. The belief that “nothing can be done about umbilical cord issues” doesn’t help because it allows providers to use the line that “these things just happen”.
If cord accidents DO happen, then why are we told they don’t? If they DON’T happen, then why are we told they do?
Why should I say anything about a cord issue?
Many families find out accidentally or after the fact that their baby had an umbilical cord issue. Most providers I talk to tell me that they will not tell families about the issue. If they do tell them or the family finds out, the provider will minimize their level of concern. Why?
Most providers say they ‘reassure’ their patients that cords don’t cause problems because they don’t want the mothers to worry and they can’t do anything about it anyway.
First – your job is not to keep me thinking that everything in pregnancy is bubblegum and unicorns. Your job is to assess me and my baby and provide your professional recommendations about how to protect us both from harm.
Second – why aren’t you the ones asking for studies to be done that would help you have treatment options?? Our medical community should be leading the charge in demanding we learn more. The advancements we have made in the last few decades in almost every area of medicine are incredible. Why isn’t stillbirth (and cord accidents in particular) one of them? The lacks of research and treatment options directly affect you, your patients, and how you practice.
Third – If you don’t know what to do about a condition or don’t feel like there are good options, tell us that! We have the right to know what is going on with our bodies and our babies. Let us be a part of that conversation. Other areas of medicine don’t get away with this.
Cords don’t get tight with labor or cause the baby to be in distress
Umbilical cords can become taught during labor depending on many forces including the length and position of the umbilical cord and the position of the baby. All the ways a cord can be compressed or compromised during the pregnancy can happen during delivery as well. Any change in physiologic status can cause fetal distress – including hypoxia secondary to cord compression. Not every baby who experiences distress during labor has a cord issue, but many do. There are other causes of distress as well, but that does not mean cords aren’t one of them.
I personally had the experience of watching my baby demonstrate this effect. While on a fetal heart monitor and having an ultrasound completed, we were able to see my baby’s position compress the umbilical cord. Within about 8-10 seconds, my baby’s heart rate started to decelerate. When she moved and the cord compression was relieved, her heart rate returned to normal. Once her heart rate began to decelerate and she was not able to relieve the compression enough for her to recover, she was immediately delivered. Because of this experience, I believe 100% that cord compression can be a cause of fetal distress.
Cesarean section is the only cure for a nuchal cord.
A newer question I have been asked is if a C-section is required to save a baby when a nuchal cord is identified. I’m going to discuss this in terms of all cord issues (not just nuchal for the reasons mentioned above). A C-section does not necessarily prevent cord issues, and it is certainly not the only way to reduce or manage cord complications. There are situations where a provider feels this gives the mom and baby the best chance of positive outcomes. I am in support of any decision made with the family for those reasons. I also believe vaginal deliveries are possible when cord issues are present. In this case, knowledge about the issue, close fetal monitoring, and access to emergency care can help provide reassurance and warning about emerging symptoms.
There are many, many complex factors that must be evaluated when making the decision to have any surgical procedure. I am not a fan of surgery whenever possible, but I also firmly believe that surgery is not the worst thing that can happen to someone. This is simply another treatment modality that can be evaluated and considered. Sometimes we must choose the lesser of evils.
Umbilical cord accidents don’t happen very often.
This is a statement made only by one who has never been affected.
And I would like to know what your definition is of the word “often”.
Stillbirth in general occurs 26,000 times every year in the United States. If we use the SCRN numbers of 11% of stillbirths being caused by umbilical cord accidents, that would indicate that 2,860 babies will be stillborn this year due to umbilical cord accidents. That is more than the number of SIDS deaths per year. That is significant.
And these are the prenatal deaths. What about the babies with umbilical cord accidents that only survive minutes or days? What about the babies who develop cerebral palsy or other conditions as a result of the hypoxia suffered during an umbilical cord accident?
Which leads me back to where we began – we need more research to understand, manage, and prevent this cause of poor pregnancy outcomes.
7 Comments
This is all very interesting ..thank you for the facts..when our grandson was born still our son inlaw came to us and said the cord was around his neck and he choked. He was very satisfied that there was an “answer” and something they couldnt do anything about… the Dr told us that probbly was the reason but this would be the only time they could have an autopsy to find out for sure or if there was any thing else to find out…our son inlaw was satisfied that they had “the answer” and didnt want to do an autopsy (for the obvious upsetting reasons) but our daughter felt the Dr was recommending and they should so they did and found out that the reason was maternal fetal hemmorhage. But for those outside the immediate family they told them the chord was around his neck. That is something for whatever reason people accept. As your article mentioned so much needs to be done to research this and hoepfully the medical and other groups will try to get answers with more researchm, but it still seems like doctors don’t push for this. I think at the least strongly suggesting autopsy can lead to more information.
My son was stillborn due to a true knot in his cord. I had US almost every week for the final 6 wks but ultrasound cannot detect a true knot in most cases. Had it been detected, my son could have been born via c section and would have lived. We need better technology as well.
This is such a great article and so true. I lost my baby girl at one day from 41 weeks during labor after a perfect pregnancy with no complications. She weighed 8 lbs. I had labored at home as directed by my doctor (it was a Sunday) until my contractions were 5 mins apart. I had never gone into labor on my own. My water did not break. I went into the hospital thinking everything was proceeding well. By the time I arrived at the hospital, my contractions were closer to 2 minutes apart. They immediately tried to use the doppler to find heartbeat and couldn’t find it. They didn’t say anything to me until my doctor arrived and hooked up the ultrasound machine and confirmed no heartbeat. We had no idea what could have happened. During delivery, my physician noted and showed my husband the cord that presented in front of her head that appeared to have been compressed. I think the risk of stillbirth from cord compression is greatly increased in late stage pregnancy (especially post-40 weeks) when babies are larger and can put more pressure on the cord and especially with the added pressure of labor. Because I went past due with both previous pregnancies and needed to be induced, I had begged our physician to not make me go so far past my due date without intervention because of the risks. I feel that the current “medical recommendations” are lacking for mom’s who go past their due dates, and that standards of care are greatly lacking. With these increased risks, we need physicians to monitor mothers and babies at this stage. Why should preterm babies receive better care than otherwise healthy full term babies who made it through the full 9 months of pregnancy? It just isn’t fair or right. I do think these statistics for cord accidents leave out many stillbirths because so many of us do not get official diagnoses or opt out of medical autopsies for official reports. Since it seemed like we knew the cause of our daughter’s death, we opted out of autopsy so we could spend our limited time with our daughter.
And I agree that if properly monitored earlier in labor through a scheduled induction, my baby would likely have been born alive either naturally or through a necessary c-section.
When I was pregnant with our subsequent pregnancy I was afraid so I searched for help. I found Dr. Jason Collins with the pregnancy Institute http://www.preginst.com/ . I found out about warning signs (increased fetal movement, hiccups, the importance of kick counts etc) and about the high probability of having a baby with a nuchal cord again. He forwarded the book the “Silent Risk” and I handed to my OBGYN, the same doctor that had delivered my other two children. She agreed to read it. She monitored me highly as directed by Dr. Collins and at 37 weeks I was induced and delivered a healthy baby girl.
Before reading his book and speaking with Dr. Collins, I believed what they told me that it was a “cord accident” and that it couldn’t be helped. I don’t believe that now. I believe I can see the double nuchal cord on the 20 week ultra sound, and the fact that this knowledge isn’t given ANY CREEDANCE is Ludacris. I blame the ignorance of medical providers and also the insurance companies as they only “cover” the expenses of 2 ultrasounds.
I pray that they “get it right.” Enough already with the empty arms.
I think that this is the first time that I have actually set “blame.” It’s hard for me to say it because it make it someone’s “fault.” Having it be an “accident” is a lot less burdensome on my and obviously other’s souls.
Brittany, I think you are justified is setting blame. You entrust yourself and your unborn baby to a specialist. You have hired that speciailist, their reputation, their expertise, their track record. And if they “fail” in perfoming their duties (care for you and safe passage for your unborn baby), then they are to blame! That specialist should be well informed regarding the risk of stillbirth and that specialsit should maintain continuing education and be up to date on the most current research on an event that has horrfic outcomes. I don’t buy it. OB/Gyns should be providing better managment, education, demanding more diagnostics tests as part of the routine prenatal tests and clinical practice guidelines to prevent stillbirths. My baby sister just lost her baby girl at 32 weeks due to cord torsion at the placenta. Devastated is all I can say! I find it in-excusable for a provider to say,”well somethime these things just happen”. Yes, ignorance of medical providers. My sister is of Advanced Maternal Age (42) and had her first baby at age 40 via c-section. Her provider did not consider her “high risk” just because she was over 40 and did not take any additional steps to monitor nor condcut additioanl testing…stating, “the insurance only paid for 2 ultrasounds”. That is negligece! As a provider, THEY call the shots, not the insurance company. You are supposed to entrust them to do the right thing in YOUR best interest and at least inform you of your options and the best course of action. I truly do not think that happened in my sisters case and more than likley yours either.