By Lindsey J. Wimmer, RN, MSN, PHN, CPNP, CPLC
Not that long ago, medicine was a profession dominated by men – including obstetrics. That has changed dramatically with more recent reports showing less than 20% of obstetricians are now men. What is interesting to me, however, is that many of the original perceptions of women and pregnancy have not changed.
There is an unwritten narrative about pregnancy that it is a condition causing women to be vulnerable, weak, helpless, and in need of protection. And their complaints or concerns must not be rational or serious. We perpetuate many of these ideas when we talk about women (or ourselves!) being ‘hormonal’ or having ‘pregnancy brain’ as a way to justify or explain less-favorable traits.
I appreciate that some actions to protect women may come from respect for the amazing feat a woman’s body is accomplishing by growing another human being. For example – offering a seat on the bus to a pregnant woman may be an act of compassion for someone whose body is needing more than usual.
But it’s very rare in our society that we respect those we consider to be suddenly weak or helpless. It doesn’t match up. An example of this is when providers say ‘we can’t go around scaring pregnant women’. This is a very common response when we encourage health professionals to talk to women about healthy pregnancy topics such as sleeping on their side or monitoring fetal movement. There is nothing kind about withholding information that could make her or her baby safer during this pregnancy! If we respect a pregnant women and don’t see her as weak, we know and trust that she is fully capable of processing any information we share.
It’s also not true because we aren’t actually afraid of scaring pregnant women. We’re happy to make sure they don’t eat cold cuts or travel to certain areas of the world. It doesn’t make sense to me which topics are ‘too scary’ and which ones aren’t.
Having worked in busy medical settings, I think a lot of the decisions come from which topics are going to lead to more questions or more work for the providers. It’s an ugly truth that health professionals are often under enormous pressure to see more patients and order less testing/treatments that drive up costs. It takes a special person to buck the ‘higher ups’ and not fall into the platitudes or old ways of thinking. It requires providers to do what our friend Dr. Barbara Toppin challenged all providers to do at Stillbirth Summit 2019 – “be as brave as our patients.”
The crazy part is – it isn’t as hard as the providers think it is going to be. Since the Stillbirth Summit, I have had conversations with several providers who told me about concepts they learned or that were reinforced at the meeting. The Summit gave them the motivation to actively change their practice. And one of the things that surprises them the most?? It was easier than they expected! It hasn’t led to really long conversations or lots of questions and additional visits. It hasn’t scared the women away. It hasn’t made more work for them. We need to be sharing these stories so the providers can be less fearful themselves.
Many women are also starting to be more assertive in these situations – especially those who have taken it upon themselves to do additional research or ask more questions. I am asked every day by pregnant women for advice on how to ‘convince’ their provider that they really are concerned or that a specific symptom is a problem. Regardless of the situation, a patient should never have to convince a health professional to take their concerns seriously! Why do we do this??
One reason might be the larger narrative that a woman who is asking for special things is considered ‘high maintenance’, ‘demanding’, or yes – ‘bossy’. Nobody wants to be seen as ‘paranoid’, ‘hysterical’, or ‘a difficult patient’. In my experience, the most ‘difficult’ patients were the ones who were the most scared, in the most pain, or the most avoided. It’s true that they may not be the most sick, but we don’t know that if we don’t take them seriously. Conversely, we often miss those who are the most sick because they are too afraid to say anything. If we are providing compassionate care, we should be reaching out and encouraging the quiet ones to be more upfront about their symptoms and concerns with us. AND – we must sit down and really listen to the others about what they are telling us.
Many providers don’t even realize that they are doing this. They may ask a question in a way that leads the patient to the ‘correct’ answer. Or downplay concerns, or tell the patient that if she is still concerned later to come back. Why would she come back if her concern isn’t legitimate now? What is going to make the same concern more problematic in a couple of days without impacting the outcome? Or we think we are being reassuring by telling them that WE aren’t concerned – as if that is more important than what she thinks or feels.
Another way we do this without realizing it is laughing off their concerns. A recent Facebook post had an upset woman asking how she should have responded when she went into the Labor and Delivery triage center concerned about her baby’s sudden, frantic, and unusual increase in movement. She said the nurse literally chuckled and said – ‘in all my years of working, no one has ever come in for too much movement.’ That is not making the patient feel welcome or showing that her concern has been taken seriously.
I have never met someone who was so bored that they decided an evening at the hospital would be a good idea. If a pregnant woman comes in for a reason, it is only because she is that concerned. That should never be laughed at.
The nurse in the above scenario then went on to say – ‘I guess we can go ahead and check it out since we’re not busy.’ Any of us would feel silly and bothersome with that type of response. What would have happened if they were busy? This mother is worried about the health of her baby, but the nurse is giving the impression that she’s more worried about how much she has to do before going home.
These types of stories are far too common. We hear them every day from all across the US. They need to stop.
The first step is to be aware. The process of self-awareness isn’t fun or easy – but it is vital to growth as a human being and a professional.
It can start small. That is how the providers started after attending the Summit. They had to first acknowledge that they could do better, and then have the strength to act on it. But it’s now bigger because they realized it wasn’t as bad as they thought it would be! That gave them the courage to try more. And it gives them the courage to share their thoughts and experiences with their colleagues – who will hopefully be able to do the same.

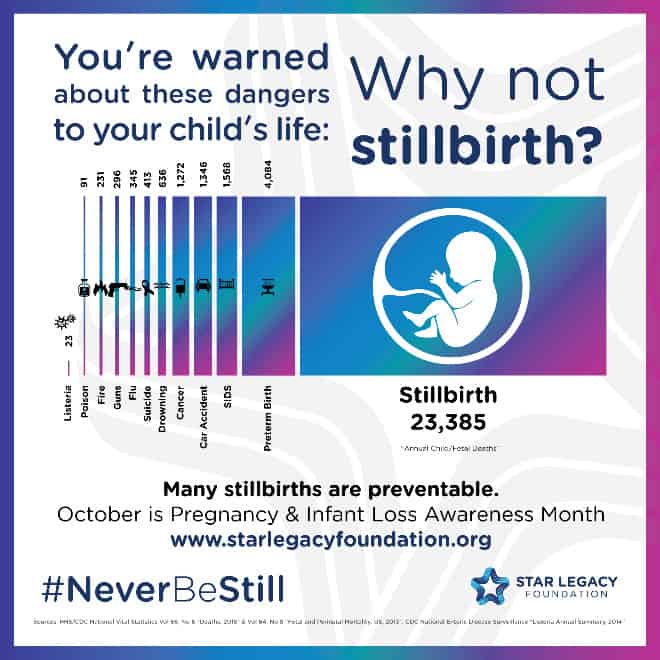
It can be overwhelming to dream of ending preventable stillbirth and neonatal death. But we start by making these small, simple steps. And that is something we can all do. I urge you to take the challenge.
Add your first comment to this post