 I was asked this question earlier this week. And it’s a very good question. There are so many conflicting thoughts, ideas, and beliefs regarding the role of the umbilical cord in stillbirth. So why is there so much confusion? And, what is the truth?
I was asked this question earlier this week. And it’s a very good question. There are so many conflicting thoughts, ideas, and beliefs regarding the role of the umbilical cord in stillbirth. So why is there so much confusion? And, what is the truth?
The truth is that umbilical cord accidents CAN cause stillbirth. There are numerous studies that have shown this to be the case. The percentage of stillbirths caused by cord accident is not as clear. Depending on the study, it can range from 5-30% of all stillbirths. The Stillbirth Collaborative Research Network (SCRN) of the NICHD recently published well-respected results from their comprehensive, 5-site study. In this paper, 11% of the stillbirths studied were attributed to cord issues. This is a significant number, but it is also likely to be a conservative number because they required physical evidence of a cord accident to be present during autopsy for this diagnosis.
 There are many types of umbilical cord issues that can cause problems. The more common issues include true knots, velamentous or marginal insertions, hyper or hypo coiling, lack of Wharton’s jelly, 2-vessel cords, and compression. Characteristics like long cords, short cords, nuchal cords, or body loops may not directly cause interruption in the blood flow, but they present a situation where compression may be more likely.
There are many types of umbilical cord issues that can cause problems. The more common issues include true knots, velamentous or marginal insertions, hyper or hypo coiling, lack of Wharton’s jelly, 2-vessel cords, and compression. Characteristics like long cords, short cords, nuchal cords, or body loops may not directly cause interruption in the blood flow, but they present a situation where compression may be more likely.
Why do so many people insist that cords (especially nuchal cords) don’t cause problems? I think it’s because most OBs and midwives have seen hundreds of healthy babies that are born with nuchal cords (the cords wrapped around the baby’s neck). This leads many people to believe that it’s not a big deal. The problem is that it CAN be a big deal for some babies. Just because it isn’t a problem for ALL babies, doesn’t mean it isn’t a problem. I know people who smoke and don’t have lung cancer. That doesn’t mean that smoking is safe. The second issue with this is that nuchal cords are just one type of cord issue that could be problematic.
Why are cord accidents difficult to diagnose? There may be physical evidence of cord compression or other type of cord accident present after birth. However, this is not always the case. Plus, many stillbirths are not evaluated by someone trained in placenta and cord pathology to identify this evidence. In fact specially trained placental pathologists are few and far between.
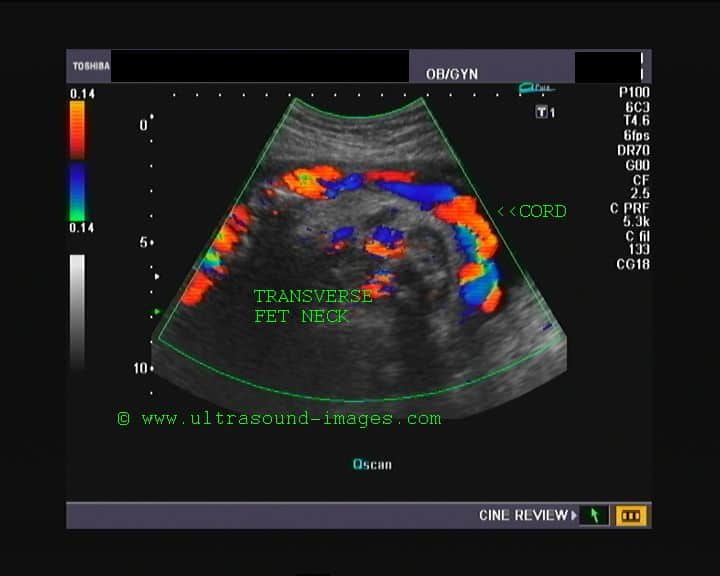
Another significant problem in diagnosis is that we lose possible evidence with delivery. It is almost impossible to know (or even guess) where the cord and all other structures were when a problem occurred if we only look at the baby and cord AFTER they have been delivered. I think all stillbirths should have a comprehensive ultrasound at the time of diagnosis to evaluate the umbilical cord, baby’s position, placental location, and amount of amniotic fluid. This is information that is impossible to determine if we don’t look at the “scene of the crime” before it has been disrupted by the birth process.
With all of these issues, why are so many parents told that an umbilical cord accident was the cause of their child’s death? This is a very good question. Anecdotally, I hear much more than 11% of stillbirths being attributed to cord accidents. Personally, I think this may be true in many of these cases. I also think it feels like an ‘easy’ answer to give parents. It is relatively simple to understand (as opposed to genetic alleles and complex medical conditions) and doesn’t appear to require a lot of explanation or proof for most families. Plus, the term ‘accident’ gives the impression that is wasn’t anybody’s fault or that it was a freak occurrence – wrong place at the wrong time type of scenario. I’ve heard people say the word accident makes it less likely the parents will blame their providers, and also that it brings a sense of closure if it’s “just one of those things”. Regardless, it should not be a default diagnosis because it’s easy. If that’s really the best educated guess of the provider, then this should be explained to the family.
I am also very irritated by the connotation that nothing can be done about issues called accidents. In many cases, there are signs or symptoms that are not identified or addressed. What these symptoms are and how they should be managed is not something I’ll get into here – but we need to start having frank discussions with expectant families and loss families about symptoms they have/had and if they could be signals of a baby in distress.
If it’s so simple, why is there so much confusion about cord accidents?? I think this is the result of the above issues in combination. During pregnancy, parents are told umbilical cords don’t cause problems. But if a loss occurs, many of these same parents are told that a cord accident is the likely cause of their child’s death. We can’t have it both ways.
How do we clear up the confusion? In my opinion, several things should happen.
- First, we need to STOP telling expectant parents that cord issues aren’t a cause for concern.
- Second, we should be encouraging families to have the baby (or at least the umbilical cord and placenta) evaluated after a stillbirth to attempt to identify the cause of death without guessing.
- Third, we need more information about how to identify these cord issues and how to manage them – this needs more research.
Until we have more research, we should be looking for signs of distress in pregnancies, and we should be looking at umbilical cord characteristics during any and all ultrasounds. If cord issues or distress are identified, the parents deserve to be told and it needs to be addressed immediately. Our OBs and midwives deserve more research and education to guide them in prevention of stillbirth from cord accidents.
With the highly sophisticated medical technology available today, I firmly believe this is a cause of stillbirth that is highly preventable! We need to work together to make it happen!
 Help us learn more about umbilical cord accidents and all stillbirths – PLEASE participate in the STARS Study and encourage others to do the same. We need women who have EVER had a stillbirth after 28 weeks gestation, women who have had a baby in the last 3 weeks, and women who are currently pregnant (28 weeks or more).
Help us learn more about umbilical cord accidents and all stillbirths – PLEASE participate in the STARS Study and encourage others to do the same. We need women who have EVER had a stillbirth after 28 weeks gestation, women who have had a baby in the last 3 weeks, and women who are currently pregnant (28 weeks or more).
Click on the logo on the left or go here to participate: https://starlegacyfoundation.org/stars1/
35 Comments
Our third daughter was born still at 37 weeks. When I presented to the hospital because I hadn’t felt her move that Saturday morning, the ultrasound didn’t show a heart beat. We were not told what they saw on the ultrasound, other than that. When I delivered her, her cord was wrapped around her neck twice (Nuchal X 2). The last trimester we had nicknamed her our “Tae Kwan Do” baby because she was so active. The night before we lost her, she was what I called violently active. But I had no idea of what was happening. I just thought I had eaten too much sugar that day or something. I hope the STARS study, which I participated in, can bring knowledge and education to the OB providers. I would strongly recommend and wonder all the time, why some type of fetal monitor isn’t offered and used during the last trimester. Also, why ultrasounds are not done more often and even weekly as you get closer to delivery. In our specific case, it was too late when we arrived at the hospital, but in many many others, if an ultrasound was a standard procedure done at the time a mother presents to the hospital, it would save babies. Cord issues would be seen right away and the necessary precautions taken at that time instead of after the mother and the baby have gone through the labor process and placed in harms way. After the loss of our daughter, I have learned of so many who had issues at the time of birth and now will have life long ailments from the cord if the baby even survived. A simple ultrasound. These are just my thoughts and opinions.
My only son was stillborn at 39 weeks due to a “cord accident” as well… When he was delivered, his cord was wrapped around his arm/shoulder, as well as his torso. He was an active baby in that last trimester, lots of hiccups and wiggling, but the day before I lost him, I too noticed a flurry of almost violent activity and kicking late on Friday night. Saturday, I’d felt very little movement, but everyone always tells you they slow down at the end anyway because they’re “running out of room.” By the time I went in to the hospital Sunday morning for lack of movement, it was also too late–His heart had stopped. He did not have an abnormally long or short cord, but he was a very large baby (9 lbs 10oz), and we think he somehow smashed his cord too tight…but that’s all we were given to understand.
I think especially…this being my first baby, I had no idea what signs to look for. I had the most simple pregnancy a woman can have. Not once was an issue raised–Ever. And then I lost him. I can say with certainty now that I will call the hospital the second I notice any slowdown in the last month if I’m lucky enough to get pregnant again. And I will be doing regular kick counts.
I also believe these issues could probably be seen through more routine ultrasounds toward the end of pregnancy. My last one had been at 36 weeks, and who knows what could have happened in those 3 following weeks? I can’t think about that now…but can only hope that more comprehensive ultrasounds and research are done to hopefully prevent this from happening to more families in the future.
I am so sorry for your loss. It is frustrating that these types of “accidents” happen. I am still so angry. This was my 3rd full term baby and I too was unaware. There is just so much that needs to change in the education of pregnancy and monitoring. So much……Again, I am so sorry for you. For us all.
I lost my boy at 38 weeks 2 days, but i didn’t understand his lack of movement was alarming. We went in to the office and my doctor couldn’t find a heartbeat. Being this late in the pregnancy and being so healthy, my doctor could only pinpoint a cord accident from low amniotic fluid. He was only 5lbs 12oz. He had a strong heartbeat… until one night. I do remember noting, he was kicking so much, so much stronger than usual. Then… nothing. This was my first pregnancy. I didn’t understand. I couldn’t do anything even if i did know. All it takes is 4-6 minutes without oxygen. we couldn’t have gotten to hospital in time if i did know. Mar. 03 is coming up quick. He would’ve been 10months+ old now.(jan2024). Every day we miss our first son together.
Thank you for sharing your story my brother just lost his baby girl at 28 weeks. The doctor said that the baby was not growing like she should. So they wanted my sister in law to go get an ultrasound to measure the baby. The doctor waited for five day then mad the appointment when the baby was born there was nothing wrong with her size or wight she was 5p 15ounces and 27in long. My bothers baby girl stopped moving the day before the appointment they went to the hospital and fond out there was no hart beat the doctor did not know why. When baby M&M was born the doctor told us that the cord was wrapped around her neck twice and that was the cause of her death It is not easy seeing your family go throw something so tragic and there is nothing you can do to help stop the pain.
I am so sorry. Cord accidents are so preventable. Its just maddening that it happens in todays world with all the technology we have available. I am so sorry about your Niece. May you and your family find some peace somehow. It is hard. Day by day. That is the best that can be.
This is a very interesting article. I wish I could go back to July 26, 2011 when I had my stillborn who was my third son. I would of have them investigate the placenta n the umbilical cord. The doctors told me it was my blood pressure but if I was on medication how could that be. My son came out of me dead yet beautiful. I want to support n e and all research because there got to be an answer. To carry a baby that far and my son was born at 30 weeks u should be happy not sad like I was.
I was wondering about this – I had a baby in Japan. He was a scheduled c-section, and part of the reason was that he was tangled in the cord. But I kept hearing American friends say that cord issues “weren’t dangerous” so I googled it. This makes me grateful for the Japanese doctors!
Thank you for your note Joy. We are aware of the differences in prenatal care in Japan thanks to the research and efforts of Dr. Hasagawa at the major teaching hospital in Tokyo. As I understand it from him, each prenatal visit includes comprehensive ultrasound in Japan to identify factors that may put the baby at risk such as cord entanglement, insufficient placental function, small for gestational age and so much more. I have NO doubt that many, many little lives have been saved because of this effort. Sadly, third trimester ultrasound in the US is not routine – but we believe it should be. We have invited Dr. Hasagawa to present his work and the Japanese prenatal protocol at the Stillbirth Summit to be held on June 19-21, 2014 in Minneapolis. (Learn more about the Summit at http://www.starlegacyfoundation.org)
Three out of four of my pregnancies had severe cord problems. Only my nuchalx2 son lived of the three. The doctor just reached in and got the cord which was wrapped around his neck twice off. He was blue and sent to the NICU right away. Thankfully he had no damage from this. My firstborn was stillborn at 40 weeks. I was awakened on a Saturday morning very early by his violent kicking. I remember thinking what in the world was THAT all about. He stopped and I went back to sleep. When I got up later, I noticed he had dropped lower in my body as I had carried him very high. I thought he was in position to be born and was so excited. Later on that day, I noticed I had not felt him move all day. I thought he was so low he couldn’t kick because I was in labor. I was out of town at the time. On that Monday, I called my doctor. I went in and their was no heartbeat. My body went limp with agony and a pain so cutting. I was treated like lets get this one out now so you can go on and have the next one. My daughter was also stillborn at 20 weeks. I noticed she had stopped kicking one Sunday night. I knew from past experience that she was dead. I went to my doctor the next morning. No heartbeat. She was born with her cord twisted at the navel like she had just swam around and around in that one spot. When she was born and I held her, she didn’t look peaceful like her brother had. Her face was full of pain. It was awful to hold her that way.
I had another pregnancy that ended in early miscarriage. All in all, I had one normal prpregnancy and birth. I was told that I produced extra long umbilical cords after my last stillbirth which was my last pregnancy.
Your story is heart breaking. So heart breaking. I am so sorry. To hear stories like this just makes me sick to my stomach. Hugs to you Gale.
Thank you for bringing this subject out in the open. One can not imagine the pain a mother goes through when a healthy baby dies at birth due to a true knot in the cord. My full term baby boy #3 died in Jan 1981. I had ultra sounds that did not detect any issue but in the last few weeks Baby Ryan would not stop moving specially if I tried to lay down to sleep at night. I saw my Dr. who dismissed my concerns and told me it was “all in my head”. Two days later, in the night, Baby Ryan died while I was asleep. In the morning I could feel the pressure in my belly had disappeared, the movement was still and I went to the ER. The Hospital staff looking after me were so shocked, they gave me another ultra-sound but they wouldn’t admit to me that my baby was dead until I delivered him a week after he died.
If this happens once to a mother she is a high risk for another event. These babies can be saved if everyone involved is trained to see the signs and knows what to do.
Lucky for me, on pregnancy #5 I had a special nurse assigned to me who saved my blue born baby girl who was strangled by the cord from death by reacting with swift knowledge and skill-full hands.
I have two healthy vibrant adult children living out of 5, I totally feel for all of you who have suffered this loss.
Many years later to understand why this happened to me I went to see a specialist who told me he could not answer why. I began to research my records from the hospital using the autopsy wording and Google search engine. This led me to a Book called “Silent Risk” and Dr. Jason Collins which helped me to understand how it happened.
I then researched my family Tree to see if there were any common factors with others in my Ancestry. I would like to see some research done on the DNA in lines that carry many Stillborns.
On Mayb31st of this year my daughter in law delivered a beautiful baby boy 7 weeks early due to cord accident. This is her second pregnancy and has been more than difficult. She suffered a severe kidney stone episode 4 days before the Dr discovered no heart rate. They felt him moving 11 pm the night before and he was gone at 8 am. Since his funeral mommy has be hospitalized for abnormal bleeding that required a d & c. One half hour before the surgery the OB Dr told them they got the placenta results back and the baby had Downs Syndrome. My kids are heartbroken. I pray for all of you that have lost your children and hope you never have this awful pain and heartbreak again.
My nephew (Blake Steven) was stillborn at 38 weeks, on April 18th 2014. He was a beautiful 8lb baby. Who looked like his mommy. He had her curly hair, and her prominent indent on her nose. My sister is the last one of her five sisters to have a baby (we all have children of our own), We are all devastated for her. We all wish we could take her pain away, especially our Mom. With reading all your stories there is one thing that sticks out at me, and it is the violent activity. She too experienced the violently kicking, prior to his death. It is now her mission (along with ours) to get a bill passed for late term comprehensive ultrasounds, so that no mommy has to hear that her baby has passed away. A sleeping giant has been awaken. We have a large family, and we will do everything we possibly can do to prevent this from happening again! We will not settle with “there is nothing we could have done to save him. It was a fluke thing.” So if their is someone who can help put this bill in motion, or knows the steps that we need to take. We would greatly appreciate the help. Our hearts go out to all of you! We will pray that you find peace within your families to get through this extremely difficult time in your lives.
I lost my baby this 17th August 2014 and that day was my birthday. One thing I found common in all the comments are baby was violently active same was the case in mine. My baby was violently active last night my wife thought it is ok, next morning when she went to the doctor , there were no heartbeat.
I have seen my cute baby lying dead. Trust me the baddest thing can happen to me in my entire life and that to my birthday.
I am emotionally not stable now.
The cord was strangled around the neck. This was my first baby.
Is there any symptoms or preventions to be taken care of ?
Please help
Last year on September 26, I lost twin girls at 21 weeks. I know this is way early than lots of you and this was my first pregnancy. My babies died due to cord entanglement plus four knots in their cords. I too noticed a couple of days before, I felt one twin move, then the other one move, like back to back, then nothing. I didnt know until I delivered them that they also shared both placenta and amniotic sac. Before this, my pregnancy was going great, no concerns. I am scared to death if I get pregnant again, if this will happen and can cord entanglement be prevented? I was told by my doctor that once cord entanglement starts theres nothing to prevent it. I cant help but still have so many questions.
Paula – I am so very sorry for your loss. It really makes no difference if the loss was early or late – the pain is still the same. You might want to get a copy of Dr. Jason Collins’ book – Silent Risk. He is the foremost authority on umbilical cord issues in the world. His book is available on Amazon.com for $19.97 or $3.99 for electronic download. It is well written and very easy for non-medical personnel to understand. You also need to give a copy to your doctor! Also, Dr. Collins is always very happy to talk to Moms – if you want to talk to him send me a note at [email protected] and I will send you his contact information.
My heart goes out to everyone who has experienced this type of loss. I lost by my daughter on Sept. 8, 2014 at 40wks due to a cord accident. My contractions had officially started and fetal monitoring the night I was in labor was “beautiful” and I was sent home because I had not dilated enough to be admitted. The accident happened sometime in between that hospital visit and the next morning when they could not detect a heartbeat. This was my first pregnancy which the doctor’s described as a “healthy…textbook pregnancy”. The loss has been devastating. Like of many of you, I am educating myself on cord injuries/stillbirths which has helped with grieving process. The open (healthcare) enrollment season (which only happens once a year at my job) has forced me to consider my healthcare needs if a subsequent pregnancy were to occur. Ladies, please ask (or demand) the care that is going to put your mind at ease. I have already had one doctor tell me that she would not treat me any different outside of “occasional” fetal monitoring in my last trimester because I had a healthy-normal pregnancy. Thankfully my personal OB has agreed to regular ultrasounds–something I plan to request upon EVERY visit; a referral to a perinatologist (a sub-specialty in OB for high-risk pregnancies); bi-weekly fetal monitoring starting at 34 weeks; and early induction options. Needless to say they don’t want me to switch but nevertheless I encourage you to ask for additional care. I’m also considering hiring a personal midwife or doula for additional monitoring/support. I’m scared to death of the trying again but I hope to find the courage one day when the time is right. I’m curious to know what other additional OB-medical care other mothers have requested after a stillbirth? Shauna- thanks for the book recommendation! Maybe Dr. Collins has some suggestions.
[…] article about the truth of the accidents with the umbilical cord it made much more sense to me. http://stillbirthmatters.wordpress.com/2013/04/05/whats-the-truth-about-cord-accidents/ For example, the doctor told us after 6 months we should write down the amounts of baby kicks ( […]
Paula – I am so very sorry for your loss. We simply have to learn as much as we can in order to advocate for our babies. I know that you will find Dr. Collins’ book very helpful. It also contains a prenatal visit protocol that he recommends. If you would like to speak to Dr. Collins personally just send me a note to [email protected] and I can provide you his contact information. He is always happy to visit with families. Shauna
[…] article about the truth of the accidents with the umbilical cord it made much more sense to me. http://stillbirthmatters.wordpress.com/2013/04/05/whats-the-truth-about-cord-accidents/ For example, the doctor told us after 6 months we should write down the amounts of baby kicks ( […]
My first baby was died on his 32 week on my tummy .
Because of twisting of cords .
What can i do to avoid this thing happen to me again .
Please give me some advice. Because its verry hard for me and my husband if this thing happen again.
From my experience the only thing that can prevent your baby from entanglement is to learn everything about the signs of when it begins to happen. My last pregnancy was perfect, I was 2 weeks overdue when my little girl became over active. I was not in labour but with persistents that this could be happening again, a wise nurse made it her mission to save my daughter’s life. That was 30 years ago. Ultrasounds made no difference, education on the nurse’s part and her quick reaction saved a healthy little girl from death. Make sure your Medical team is well educated about cord related accidents and methods to prevent death. Persist when you know something is wrong. Be brave as the end results are well worth it. 🙂
[…] about the truth of the accidents with the umbilical cord it made much more sense to me. http://stillbirthmatters.wordpress.com/2013/04/05/whats-the-truth-about-cord-accidents/ For example, the doctor told us after 6 months we should write down the amounts of baby kicks ( […]
I was told reaching up over your head can make the umbilical card wrap around your child’s neck, is this true?
This is a common myth – but it has absolutely no basis in science. Women should not be concerned that their movements cause or prevent umbilical cord wraps.
My daughter recently lost her baby at 17 weeks. When she gave birth the nurse stated that the cord was wrapped around his neck very tightly. The post mortem showed this to be the cause of his death. She is currently searching for reasons as to how and why this happened.
[…] article about the truth of the accidents with the umbilical cord it made much more sense to me. http://stillbirthmatters.wordpress.com/2013/04/05/whats-the-truth-about-cord-accidents/ For example, the doctor told us after 6 months we should write down the amounts of baby kicks ( […]
My daughter also lost her baby. She had a normal pregnancy.It was at the time she was having contractions where things went wrong. She was having contractions and went to the hospital but they sent her home saying to come back when she was having the contractions 2 minutes apart. The next day she went back to the hospital but her doctor wasnt there,so they gave her a shot to try and stop the contractions, sent her home again and told her to go to het schedulled appointment at her doctors office. The next day when she went to her appointment and the doctor looked at her, the baby was akready crowning and they haf to quickly get the bby out then and there. When the baby came out he wasnt breathing. They tried to get the baby to breath but to no avail. The doctor said it was because the umbilicle cord got wrapped around the babies neck but they checked the placentia and the umbilical cord everything looked fine. This ws my daughters first child. I think maybe it was the shot that caused her to lose her baby but im not sure. What do yoy think?
My baby died at the age of 35 weeks of gestational age before entering OT due to entanglement of umbilical cord in its wrist.this was our first baby. What we should do to avoid it in the next pregnancy.
I realize this is an old post, but it was oddly encouraging. We lost our firstborn daughter at 39 weeks to a cord accident. People tell you this doesn’t happen and that you “don’t need to worry” about nuchal cords before birth. That most times, doctors won’t even mention them because they just cause worry for the parents. Just here to say we are a clear statistic. We went for concerns about our baby girl’s movement and there wasn’t a heartbeat. She was a bigger baby (8 lbs 4 oz) and extremely active. We had a long umbilical cord from what I was told, measuring 75 cm (normal is around 50 cm). She had a tightly wrapped triple nuchal cord upon delivery and there was nothing else wrong with her. We are currently 33 weeks pregnant with our second baby now and have a scheduled induction at 39 weeks. I am doing weekly ultrasounds and my new OB is actually checking on the umbilical cord each week to see as much as possible. I am acutely aware of kick counts and checking heart rate often for any signs of distress. My doctors have all told me that nuchal cords are not recurring and neither is umbilical cord length the same each time. Thankful for the precautions they are taking with this pregnancy. I do think nuchal cords/umbilical cords need to be investigated more throughout pregnancies in general and less talked about in nonchalant ways by doctors.
Hi Amanda. I know your comment was from last year but it was the most recent one in this thread. We just lost our sweet boy at full-term 40 weeks on his due date Nov. 26th 2021 to a quadruple Nuchal cord accident. I too also had an abnormally long cord which was attributed to him “stretching the cord” from being so active. I feel so foolish and stupid because I had been asking about his activity for weeks, if it was normal how much he moved around and how active he was. “Should I be concerned?”. I was planning for a home-birth delivery . He was wild since he was able to move, which his older brother is just as wild so I was suspicious but didn’t expect anything to be wrong because I was constantly told that it is a sign of a healthy baby. This thread is so sad, but it has ignited a fire under me to try and change this stigma that still happens, almost 10 years later from when this article was originally written. I will not let my sons death be in vain. I am so happy to hear about your second pregnancy and that your doctors are being diligent and taking your concerns seriously. I hope you had an easy pregnancy with your second and I wish I was able to contact you directly as a support person and friend during this time. Thank you to all the ladies for their stories of loss, I grieve along with all of you. This is not a club that anyone should be in, if it is preventable. I miss my son terribly. My husband and I are absolutely shattered. I hope everyone here recovered and I hope to hear from Shauna as well to try and gather information on how to advocate for change. I bought the book and will be looking up Dr. Hasagawa in Tokyo. If anyone wants to contact me, feel free to email me at [email protected]
I was 34 weeks when I found out the cord was wrapped around my child’s foot. I had an ultrasound and 4D ultrasound two weeks before this happened and my next appointment to see OB was to weeks later. My baby was pretty active and love kicking under my breast. Then the next day I didn’t feel him and I thought nothing of it because sometimes he does that. I’ve been the the hospital twice before this because I didn’t feel him but he was still okay. The next morning I went to the hospital because he didn’t move all day. I even ate some candy just to make sure. They hooked me up to the monitor and said I think your heartbeat is going with his then they pulled out the ultrasound and told me the most horrible news that my baby has no heartbeat. Most heartbreaking three days of my life. I did a natural delivery with epidural to get him out. I didn’t hold him or look at him it was so painful. My doctor who delivered him said the next time you get pregnant starting at 30 weeks you need to get seen twice a week. But he said it’s a rare thing. In two days I’m gonna bury my child. I’m very angry that I wasn’t seen enough.
My daughter was born still at 31 weeks. I went to the hospital at 28 weeks because I noticed she wasn’t being active. Hospital tells me everything is okay. But my fluid levels should be at a 10cm and I was at a 9.5cm. I later found out also that the tech saw the nuchal cord and did not inform me. At 30 weeks I have a 4D I was told my water levels looked low I should see my doctor. I went to my doctors office the following day telling them what I was told. They told me they don’t take medical advice from people that only take pictures. I told them to please check me. They sent me home telling me everything was fine. 2 days later I’m rushing to the hospital because my daughter hasn’t moved in 2 hours. She was gone with fluid levels at 1.9cm and when delivered her cord was wrapped around her neck. The doctor decided to put on her death certificate that I was a cord accident. Never wanting to address the little to none amniotic fluid.
We lost our daughter at 38 weeks. She was very active during whole pregnancy and I noticed that she stop being active on Saturday. I felt her stretching but went to OB Monday. They checked heart beat, said it was strong and I was informed babies don’t move much in the last weeks due to lack of space. I am devastated because I didn’t feel movements after that and I was under impression that she has no room. My belly drop and we thought with my husband that she is getting ready for the delivery. I am in so much pain that I should have gone to hospital. When I went for next appointment there was no heartbeat anymore.